2024
INDUSTRY TRENDS REPORT
Comparing Workers’ Compensation – Examining PT Outcomes within the Broader Health Care System
Each year in the United States, approximately 300 million physical therapy sessions are conducted to aid patients in injury recovery.i The increasing use of PT services is attributed to various factors, notably the growing body of evidence demonstrating that greater reliance on physical medicine helps to mitigate healthcare expenses in other areas.
Utilization of physical medicine services often coincides with a reduction in surgical interventions, the use of prescription medication, as well as shorter hospital staysii. Outside of workers’ compensation, the broader healthcare market is prioritizing PT care and removing barriers to help patients increase the ‘Speed to PT Care.’
In the 2024 Industry Trends Report, MedRisk examines data from the broader healthcare market to see where the use of PT over alternative treatments is delivering positive clinical and economic benefits and what we can learn by looking at our own data.
What We Can Learn from the Broader U.S. Healthcare System
Within the U.S. healthcare system, we’re seeing an increased focus on the speed to provide physical therapy services to patients. Group health and government-sponsored programs alike are making it easier for patients to visit physical therapists promptly.
Mounting Evidence Indicates that Direct and Faster Patient Access to PT Improves Outcomes
According to new research from the Department of Defense (DoD), direct access to physical therapy improves patient outcomes and reduces costs. The study conducted at Joint Base Lewis-McChord credits better cost and health outcomes for patients seeing PT first for musculoskeletal care.
Recognizing the benefit of getting patients to physical therapist services as soon as possible after injury, UnitedHealthcare launched a pilot program aimed at increasing access to physical therapist services to encourage patients to seek more conservative care routes for lower back pain.
Use of Physical Therapy Services Delivers Positive Health and Economic Benefits to Patients Over Other Treatments
A groundbreaking independent, evidenced-based study commissioned by the American Physical Therapy Association (APTA) examined condition-based physical therapist services to determine the health and economic impact of physical therapy over alternative treatmentsiii.
This landmark study – conducted outside of workers’ compensation – found PT delivers significant clinical and economic outcomes over alternative treatments across multiple conditions, including in three common workers’ compensation injuries: carpal tunnel syndrome, low back pain and lateral epicondylitis (also known as tennis elbow).

Reported Savings Per Episode of Care When Using Physical Therapy Over Alternative Treatments:
$39,533
CARPAL TUNNEL SYNDROME (CTS)
Net Economic Savings
$4,160
Low Back Pain
Net Economic Savings
$10,739
LATERAL EPICONDYLITIS
Net Economic Savings
Where medically appropriate, the study quantifies that more widespread use of PT services can deliver improved health and economic benefits.iv

10 Year Look Back: Across All Injury Types ‘Speed to PT’ Stalls
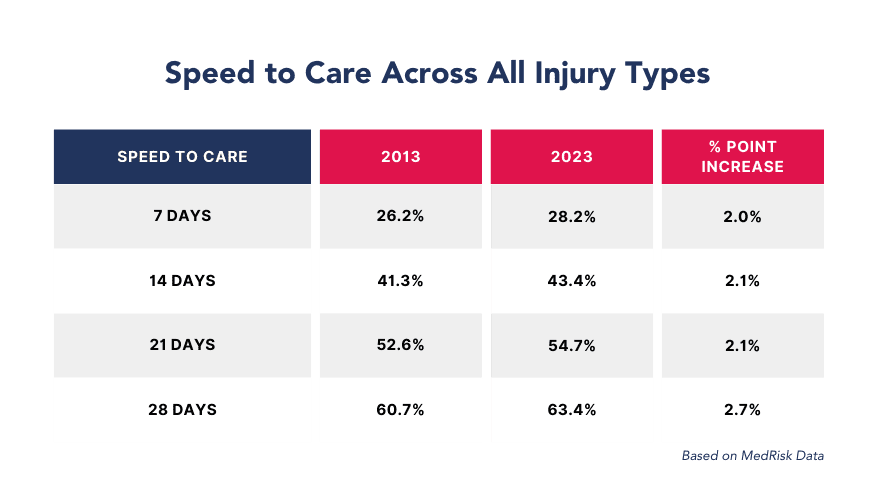
Despite an abundance of evidence that earlier PT involvement is better for recovery outcomes, there has not been a significant change in the speed of getting a patient to PT (calculated from DOI to first treatment date) over the past decade across all injury types.
Speed to Care rates have only increased approximately two percentage points over the past ten years. Increasing speed to care by encouraging earlier access to PT treatment may provide positive health and financial outcomes in workers’ compensation claims.
In Workers’ Compensation, Speed to Care Lags in these Three Conditions
127 Days
Speed to Care for CTS Claims
Carpal tunnel syndrome (CTS) is related to repetitive hand movements commonly occurring in production workers and administrative staff when there is compression of the median nerve at the wrist, specifically the carpal tunnel.
Use of physical therapy services over surgery for CTS has been shown to improve patient quality of life by reducing pain and improving function and nerve conductionii. At 127 days to initiate PT care, there is a significant opportunity to increase speed to care to impact claim outcomes.
61 Days
Speed to Care for Lower Back Pain
Back pain is a leading cause of work-loss days as well as limitationsv and is a common workers compensation injury. With an incidence rate of 20 per 10,000 full-time workers, and an average of 7 days away from work per injury, low back pain is a leading cause of acute care visits for work-related injuries.vi, vii
While many cases of acute low back pain (lasting less than four weeks) resolve without intervention, one in three patients still have symptoms a year after an episode of low back pain.iv
74 Days
Speed to Care for Lateral Epicondylitis
Commonly referred to as tennis elbow, lateral epicondylitis, is caused by an overload of the extensor carpi radialis brevis tendon stemming from overuse or repeated gripping.
Despite its name, only 10% of the patient population is comprised of tennis players. As many as 15% of workers in highly repetitive jobs report having tennis elbow.
Carpal tunnel syndrome, low back pain and lateral epicondylitis are three musculoskeletal injuries that respond well to PT, and for which an abundance of evidence suggests that non-surgical care is effective, especially when PT care occurs soon after injury.
Within the workers’ compensation market, we have the opportunity to improve the average speed to care (calculated as time between date of injury and date of PT care) to help improve claim outcomes.
Psychosocial Barriers to Recovery
It’s not just the injury or speed to care that’s impacting health outcomes. Psychosocial factors have an impact on claim outcomes as well.
One way to predict long-term disability and work absenteeism in injured employees with acute and chronic musculoskeletal pain from soft tissue injuries is by using the Örebro Musculoskeletal Pain Screening Questionnaire (ÖMPSQ). This screening tool is used throughout the healthcare system – both in workers’ compensation and other health plans.
ÖMPSQ identifies psychosocial and functioning-related risk factors among individuals with musculoskeletal pain and classifies individuals as low, medium or high risk.
Using the ÖMPSQ to screen injured employees, MedRisk found a correlation between the patient’s risk score and the total number of visits required to treat their injury.

Örebro Score at First Screening
The Örebro Risk Score provides early insight to claim risk and the opportunity to intervene, as appropriate, to support positive claim outcomes.
At the first screening, injured employees’ risk scores are fairly evenly distributed among low, medium and high risk, with slightly more than a quarter of injured employees categorized as high risk.
PT Visits by Örebro Score at First Screening
There is a direct correlation between the injured employee’s risk score at first screening and their total number of PT visits.
Injured employees with medium Örebro risk scores on the first screening had a 22% increase in the total number of PT visits compared to injured workers categorized with low-risk scores, increasing to a 27% increase for those individuals with a high-risk score at first screening.

Digital MSK Solutions:
A Mini-Guide for PT
In addition to addressing Speed to Care and psychosocial components of claims, payers and providers are also reviewing new tools to enhance therapeutic outcomes.
The workers’ compensation landscape is teeming with new digital tools promising to revolutionize injury recovery. With new players emerging constantly, it’s easy to feel overwhelmed and unsure where to even begin. This mini-guide aims to equip you with a framework to think about these tools in broad categories, helping you identify those most relevant to your needs.
Before we dive in, it’s crucial to understand that currently, there’s no definitive evidence proving these tools directly impact recovery time within the U.S. workers’ comp system. While related studies offer promising hints, these tools shouldn’t be seen as a guaranteed “fast-track” to returning to work.
Categorizing the Digital MSK Toolbox
Categorizing digital MSK solutions grants you the power to quickly grasp each tool’s purpose (support, supplement, or substitute) and its potential impact on the recovery journey. Need to compare features or costs? Categories make it a breeze. Ultimately, understanding these categories empowers you to make informed decisions about which tools might best fit your program as a whole and offer maximum effectiveness.
Let’s explore the three main categories
Support
These tools focus on streamlining the injured worker recovery process. They support the patient and provider as they navigate the industry’s existing recovery framework providers.
Enhancing Provider Capabilities: The use of software and hardware to aid clinicians in assessment (ex: assessing mobility, strength, function) and designing and enhancing treatment plans.
Enhancing Patient Experience: The use of technology to support the patient through the recovery process. Apps to support mental health, guide independent exercise programs and promote self-care can empower patients and improve their engagement in recovery.
Supplement
These tools aim to expedite recovery while working alongside the existing rehabilitation model.
Enhanced Self Care: The use of motion tracking apps and wearable devices during independent exercise can drive compliance and provide real-time performance feedback to the patient and provider. Virtual reality tools offer an immersive environment for addressing a variety of concerns including pain, anxiety and restricted mobility.
Telerehabilitation: Platforms allowing patients access to rehab professionals between, or in lieu of, in-clinic sessions allow for greater patient engagement and continuity of care.
Substitute
(Limited Application)
While still in its early stages, some tools aim to partially replace certain aspects of clinical care.
Tech-assisted assessment includes the use of hardware and AI-powered software to evaluate musculoskeletal conditions and generate care plans (typically independent exercise programs).
Tech-assisted self-care guidance includes the instruction and monitoring of exercise programs using motion-tracking apps and/or sensors.
Why Research Matters
The workers’ compensation landscape, as we’ve shown, is ripe with opportunities to optimize for both financial and medical success. Progress thrives on out-of-the-box thinking, and we’ve pinpointed key areas where collective action can show its full potential. Through collaboration, we can not only achieve improved financial results but also accelerate patient recovery, paving the way for a collective win.
At MedRisk, we’re constantly delving into research, analyzing data, and leveraging our long-standing expertise to turn these possibilities into concrete solutions for our valued customers and partners.
MedRisk by the Numbers
MedRisk is the leading provider of managed physical medicine for the workers’ compensation industry and related market sectors. While we provide individual care to over half a million patients each year, we also measure our outcomes in aggregate so we can report on our results and trends. Here’s a closer look at MedRisk based on 2023 data:

Injured Workers Treated by MedRisk Providers
150k+
Total Network Providers in MedRisk Network
iIBIS World, 2022. iiNational Institutes of Health, National Library of Medicine. 2023. iii, ivThe Economic Value of Physical Therapy in the United States. American Physical Therapy Association, 2023. vGeorgetown University Health Policy Institute, McCourt School of Public Policy. Chronic Back Pain. viHoy DG, Smith E, Cross M, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis 2014; 73:982–989. viiNonfatal Occupational Injuries and Illnesses Requiring Days Away From Work, 2015. Accessed September 5, 2018. viiiThe Association between Early Opioids Prescribing and the Length of Disability in Acute Lower Back Pain: A Systematic Review and Narrative Synthesis.